A 20 year old female came to casualty with complaints of loose stools and back pain
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome. I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CHIEF COMPLAINTS:-
Back pain since 2 days
Loose stools since 2 days
HISTORY OF PRESENTING ILLNESS:-
Patient was apparently asymptomatic 4 years back, then she developed irregular menstrual cycles for which she visited gynaecologist and was diagnosed with PCOS.
2 days back she developed lower back pain, intermittent in nature, complaints of sharp pain, which was radiating to umbilicus only from left side.
Since 2 days she was having loose stools, watery in consistency, 4 - 5 episodes and it is not associated with blood stains.
2 days back she also had 1 episode of vomiting, which contains food particles and is non projectile in nature.
No history of fever, SOB, headache.
No history of outside food intake.
PAST HISTORY:-
No history diabetes mellitus, Hypertension, epilepsy, TB, asthma, thyroid abnormalities.
PERSONAL HISTORY:-
Diet- decreased
Sleep- not adequate
Appetite- decreased
Bowel and bladder movements- loose stools
Addictions - nill
No allergies.
DAILY ROUTINE:-
She is a final year student of B.SC nursing living in hostel.
She wakes up at 5:30 am does breakfast at around 6 am and catches bus to Nalgonda at 6:30am
She reaches to Nalgonda and starts her duty at 8 am and finishes by 1:30pm.
She returns to her hostel and consumes lunch at 3 pm and after that she takes rest for 2 hours.
She eats dinner at 7:30pm or she skips dinner sometimes.
She does her work from 8 pm to 2 am and then goes to sleep.
MENSTRUAL HISTORY:-
Age of menarche:- 15 years
Menstrual cycle:- 5 days / month filling 7 pads per day.
LMP - in October ( 3 months back )
Diagnosed with PCOS 4 years back.
TREATMENT HISTORY:-
No significant treatment history.
FAMILY HISTORY:-
No significant family history.
GENERAL EXAMINATION:-
Patient is conscious, coherent, cooperative and well oriented to time, place and person
Moderately built and moderately nourishment.
Vitals :-
Temp - afebrile
BP - 120/80 mm/hg
Pulse rate - 86 bpm
Respiratory rate - 13 cycles per minute
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy - absent
Oedema - absent
SYSTEMIC EXAMINATION:-
1) abdominal examination:-
Tenderness over the umbilical region and left lumbar region which was radiating from back on left side.
No organomegaly
No shifting dullness
No fluid thrill
Bowel sounds not heard .
2) CVS examination:-
- S1 S2 heard
- no murmur heard.
3) Respiratory examination :-
- Chest bilaterally symmetrical, all quadrants
moves equally with respiration.
- Trachea central, chest expansion normal.
- Resonant.
- Bilateral equal air entry, no added sounds heard.
4) CNS examination :-
- No focal neurological defects.
- all cranial neves are intact.
GCS:- 15/15
Power:-
Rt UL-5/5. Lt UL-5/5
Rt LL-5/5. Lt LL-5/5
Tone:-
Rt UL -N
Lt UL-N
Rt LL-N
Lt LL-N
Reflexes: Right Left.
Biceps. ++. ++
Triceps. ++ ++
Supinator. ++ ++
Knee. ++ ++
Ankle. ++ ++
Plantar: Flexion Flexion
PROVISIONAL DIAGNOSIS:-
Acute gastroenteritis .
INVESTIGATIONS:-
Ultrasound :-
ECG:-
Random blood sugar:-
Complete urine examination:-
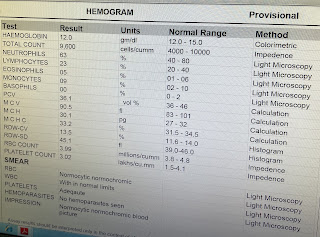
Hemogram:-
LFT:-
RFT:-
TREATMENT:-
Inj METROGYL 500mg IV/ TID
Inj. PAN 40mg IV/ OD
Inj. ZOFER 4mg IV/ OD
Tab. ULTRACET PO/ BD
Inj. CIPROFLOXACIN 200mg IV/ BD
IV fluids NS @ 100ml / hour
Tab. SPUKLAC DS PO / TID
ORS sachets in 1 liter of water - 200ml after each episode of loose stool.









Comments
Post a Comment