Case based OSCE along with BLOOM’S learning levels Achieve
4)Case based OSCE along with BLOOM’S learning levels Achieved
This is an online e log book to discuss our patient identified health data shared after taking his/her guardian signed informed consent. Here we discuss our individual patient problems through a series of inputs from available global online community of experts with a aim to solve those patients clinical problem with collective current best evidence based inputs.This blog also reflects my patient centered online learning portfolio and valuable inputs on the comments box is welcome.I have been given this case to solve in an attempts to understand the topic of patient clinical data analysis, to develop my competency in reading and comprehending clinical data including history, clinical finding, investigation.
PERSONAL HISTORY-
Diet- mixed
Appetite- normal
Sleep- adequate
Bowel and bladder movements- regular
No known allergies
Addictions- used to consume pan one or twice daily but stopped from past 4 months.
FAMILY HISTORY- not significant
GENERAL EXAMINATION-
patient is conscious, coherent, cooperative. Well oriented to time , place and person, moderately built and moderately nourished
Vitals -
BP- 130/80 mmHg
PR- 92 bpm
RR- 18 cpm
TEMP- 98.2 F
PRESENCE OF PALLOR.
NO SIGNS ICTERUS, CYANOSIS, CLUBBING, LYMPHADENOPATHY, OEDEMA.
SYSTEMIC EXAMINATION-
1) CVS- S1, S2 heard, no murmurs.
2) RS- BAE present, NVBS
3) PER ABDOMEN- diffuse tenderness
no organomegaly
4) CNS:
Higher mental functions - intact
Cranial nerves - intact
Motor examination - normal
Sensory examination:Normal
No meningeal signs
INVESTIGATIONS-
CHEST X-RAY-
1/10/23
7/10/23
PROVISIONAL DIAGNOSIS-
PYREXIA UNDER EVALUATION WITH LEFT LOWER ZONE COLLAPSE.
PRE RENAL ACUTE KIDNEY INJURY.
HYPOKALEMIA SECONDARY TO GE , KNOWN CASE OF HTN SINCE 2 YEARS.
TREATMENT-
1. INJ. PAN 40MG IV/OD
2. INJ. ZOFER 4MG IV/OD
3. IV. FLUIDS - 2NS @ 75ML/HR
- 1 RL
4. INJ. NEOMOL 1GM IV/SOS
5. TAB. DOLO 650MG PO/TID
6. SYP. ASCORIL-LS 15ML/PO/TID.
[02/10/23, 10:01:09 PM] sowmika marru: Date- 3/10/23
ICU
Unit-6
Date of admission 30/9/23
S- c/o fever since 5 days
O- on examination, patient is conscious, coherent, cooperative.
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, oedema.
Vitals-
Bp- 130/90mmhg
Temp- 98.2 F
PR- 77 bpm
RR- 17cpm
CVS - s1, s2 heard
RS - BAE present, NVBS
P/A- diffuse tenderness
CNS -
Higher mental functions - intact
Cranial nerves - intact
Motor examination - normal
Sensory examination:Normal
No meningeal signs
A-
PYREXIA UNDER EVALUATION WITH LEFT LOWER ZONE COLLAPSE.
PRE RENAL ACUTE KIDNEY INJURY.
HYPOKALEMIA SECONDARY TO GE , KNOWN CASE OF HTN SINCE 2 YEARS.
P -
1. INJ. PAN 40MG IV/OD
2. INJ. ZOFER 4MG IV/OD
3. IV. FLUIDS - 2NS @ 75ML/HR
- 1 RL
4. INJ. NEOMOL 1GM IV/SOS
5. TAB. DOLO 650MG PO/TID
6. SYP. ASCORIL-LS 15ML/PO/TID.
[05/10/23, 1:23:36 PM] Himaja PGY1: Sir amc fourth bed
[05/10/23, 1:24:12 PM] Himaja PGY1: Aki is in increasing trends sir not responding to fluids
Stool for occult blood positive
Symptoms are not subsiding
[05/10/23, 1:24:20 PM] Himaja PGY1: Sputum for AFB turned out negative
[05/10/23, 1:24:34 PM] Himaja PGY1: I am worried are we missing on something
[05/10/23, 1:24:47 PM] Himaja PGY1: @919989643309 post the fever chart here please
[05/10/23, 1:31:48 PM] Devendra 2018: This message was deleted by admin Himaja PGY1.
[05/10/23, 1:42:00 PM] Himaja PGY1: Investigation chart photo aswell
[05/10/23, 2:11:59 PM] Rakesh Biswas Sir GM HOD: Sharing patient identifiers in social media!! 🧐😳😨👺
First time I saw Picasso drawing our fever charts!!
Where are the data points!!
[05/10/23, 2:13:09 PM] Rakesh Biswas Sir GM HOD: It's clear as daylight!
[05/10/23, 2:15:30 PM] Rakesh Biswas Sir GM HOD: Share it again asap!!
[05/10/23, 2:15:35 PM] Himaja PGY1: Mycobacterium?
[05/10/23, 2:17:07 PM] Rakesh Biswas Sir GM HOD: In the case report has @919100206300 left out the patient's HRCT chest images or was it another patient?
Also the uploaded LFT there doesn't match the LFTs in the fever chart!
[05/10/23, 2:17:18 PM] Himaja PGY1: We haven’t got HRCT done sir
[05/10/23, 2:18:15 PM] Rakesh Biswas Sir GM HOD: Which patient's was that who had a right lower lobe apical bronchopulmonary segment consolidation? <This message was edited>
[05/10/23, 2:19:17 PM] Himaja PGY1: This patient sir
[05/10/23, 2:19:29 PM] Devendra 2018: This message was deleted.
[05/10/23, 2:20:18 PM] Himaja PGY1: Please crop the identifies
[05/10/23, 2:20:22 PM] Rakesh Biswas Sir GM HOD: 🧐😳😨👺
[05/10/23, 2:21:00 PM] Rakesh Biswas Sir GM HOD: 👆
[05/10/23, 2:21:16 PM] Himaja PGY1: <attached: 00000037-PHOTO-2023-10-05-14-21-16.jpg>
[05/10/23, 2:21:23 PM] Himaja PGY1: This patient sir
[05/10/23, 2:21:25 PM] Devendra 2018: <attached: 00000039-PHOTO-2023-10-05-14-21-25.jpg>
[05/10/23, 2:21:31 PM] Himaja PGY1: <attached: 00000040-PHOTO-2023-10-05-14-21-31.jpg>
[05/10/23, 2:21:44 PM] Himaja PGY1: <attached: 00000041-PHOTO-2023-10-05-14-21-44.jpg>
[05/10/23, 2:23:45 PM] Rakesh Biswas Sir GM HOD: No I don't think so and in response to questions like that you are supposed to share the patient's case report or PaJR link not their chest X-rays as this way you are corrupting the data in this PaJR!!
[05/10/23, 2:24:28 PM] Himaja PGY1: Sorry sir
[05/10/23, 2:24:56 PM] Rakesh Biswas Sir GM HOD: Delete from here if it's not this PaJR
[05/10/23, 2:25:06 PM] Rakesh Biswas Sir GM HOD: Delete from here if it's not this PaJR
[05/10/23, 2:25:12 PM] Rakesh Biswas Sir GM HOD: Delete from here if it's not this PaJR
[05/10/23, 2:25:14 PM] Himaja PGY1: This PaJR sir
[05/10/23, 2:25:19 PM] Himaja PGY1: All the x rays
[05/10/23, 2:26:47 PM] Rakesh Biswas Sir GM HOD: Then what about the one in the DP? Who's is that?
[05/10/23, 2:27:17 PM] Himaja PGY1: This is from time of admission sir
[05/10/23, 2:27:29 PM] Himaja PGY1: This was taken yesterday
[05/10/23, 2:27:30 PM] Rakesh Biswas Sir GM HOD: Please mention the dates
[05/10/23, 2:28:02 PM] Himaja PGY1: 30-09-2023
[05/10/23, 2:28:14 PM] Himaja PGY1: 04-10-2023
[05/10/23, 2:28:18 PM] Rakesh Biswas Sir GM HOD: I remember asking for right lateral but they have repeated left lateral and written right on the chest X-ray
[05/10/23, 2:28:21 PM] Himaja PGY1: 04-10-2023
[05/10/23, 2:28:30 PM] Rakesh Biswas Sir GM HOD: And the DP?
[05/10/23, 2:29:44 PM] Rakesh Biswas Sir GM HOD: Liver ultrasound video??
[05/10/23, 2:29:56 PM] Rakesh Biswas Sir GM HOD: History of alcohol intake?
[05/10/23, 2:31:42 PM] Rakesh Biswas Sir GM HOD: Daily stool output? Weight? Images?
[05/10/23, 2:31:56 PM] Rakesh Biswas Sir GM HOD: Urine intake output?
[05/10/23, 2:32:09 PM] Himaja PGY1: No history of alcohol intake sir
[05/10/23, 2:32:18 PM] Rakesh Biswas Sir GM HOD: Share the fever timeline again with all the above data asap
[05/10/23, 2:32:18 PM] Himaja PGY1: 2200/1800
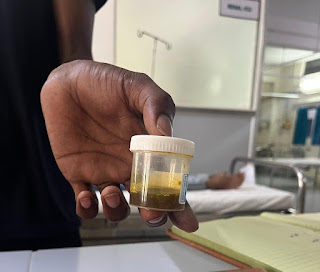
[05/10/23, 2:32:47 PM] Himaja PGY1: <attached: 00000065-PHOTO-2023-10-05-14-32-47.jpg>
[05/10/23, 2:32:50 PM] Rakesh Biswas Sir GM HOD: We want to know everyday's since admission along with creatinine
[05/10/23, 2:33:41 PM] Rakesh Biswas Sir GM HOD: This is just one small sample. What did we buy that glass jar for along with the electronic weighing machine!?
[05/10/23, 2:34:24 PM] Rakesh Biswas Sir GM HOD: Rakesh Biswas Sir GM HOD changed this group's icon
[05/10/23, 2:34:41 PM] Prachathan Sir Pg: Devendra 2018 added Prachathan Sir Pg
[05/10/23, 2:35:40 PM] Rakesh Biswas Sir GM HOD: Make me admin
[05/10/23, 2:39:42 PM] Rakesh Biswas Sir GM HOD: 👆
[05/10/23, 2:39:47 PM] Rakesh Biswas Sir GM HOD: 👆
[05/10/23, 2:40:07 PM] Himaja PGY1: @919989643309 please help to post the fever chart again
[05/10/23, 2:40:13 PM] Himaja PGY1: Without the identifiers
[05/10/23, 2:40:38 PM] Rakesh Biswas Sir GM HOD: He'll need another thirty days
[05/10/23, 2:45:11 PM] ~ Mikhitha Reddy: ~ Mikhitha Reddy joined using this group's invite link
[05/10/23, 2:43:01 PM] Himaja PGY1: <attached: 00000077-PHOTO-2023-10-05-14-43-01.jpg>
[05/10/23, 2:43:24 PM] Himaja PGY1: He is plotting it again sir
[05/10/23, 2:43:26 PM] Himaja PGY1: On a new one
[05/10/23, 2:44:09 PM] Rakesh Biswas Sir GM HOD: Either way what is clear as daylight here is that the patient is having multisystem involvement including hepatic inflammation, non oliguric renal failure and post admission post antibiotic associated diarrhoea.
We need to continue supportive therapy amidst all the differentials of viral, bacterial, protozoal etc
Leptospira, Ricketssia are commonly well known here to cause this other than viruses
[05/10/23, 2:44:57 PM] Rakesh Biswas Sir GM HOD: Ask him to add the daily intake output to it
[05/10/23, 2:45:19 PM] Rakesh Biswas Sir GM HOD: From Picasso to Rembrandt!
[05/10/23, 2:45:41 PM] Rakesh Biswas Sir GM HOD: 👆
[05/10/23, 2:53:10 PM] ~ Madeeha Abrar: ~ Madeeha Abrar joined using this group's invite link
[05/10/23, 2:55:42 PM] ~ Shiv Deshmukh: ~ Shiv Deshmukh joined using this group's invite link
[06/10/23, 9:07:55 AM] Lohith Sir Pg Gm: Lohith Sir Pg Gm joined using this group's invite link
[06/10/23, 12:00:23 PM] Devendra 2018: <attached: 00000087-PHOTO-2023-10-06-12-00-23.jpg>
[06/10/23, 12:00:23 PM] Devendra 2018: <attached: 00000088-PHOTO-2023-10-06-12-00-23.jpg>
[06/10/23, 1:02:29 PM] Prachathan Sir Pg: @919121046928 sir can it be salmonella infection
[06/10/23, 2:00:49 PM] Swathi 2018: Swathi 2018 joined using this group's invite link
[06/10/23, 2:04:15 PM] Rakesh Biswas Sir GM HOD: It can be
Viral
Bacterial
Protozoal
Which one can be found out if the organism is grown
[06/10/23, 2:59:26 PM] Rakesh Biswas Sir GM HOD: Rakesh Biswas Sir GM HOD changed the group name to “65F FEVER SINCE 5 DAYS , Telangana PaJR”
[06/10/23, 2:59:51 PM] Rakesh Biswas Sir GM HOD: Stool output and pea soup image today?
[07/10/23, 9:43:02 AM] Rakesh Biswas Sir GM HOD: Update?
[07/10/23, 9:56:39 AM] Prachathan Sir Pg: Sir pt is having continuous fever spikes with normal leucocye count
Pt is having tachypnoea with RR of 30-34 cpm
Pt is having decreased urine output since yesterday
I/O-2300/300
Today:
Sr creat-3.1
B urea-109
[07/10/23, 9:57:14 AM] Prachathan Sir Pg: <attached: 00000096-PHOTO-2023-10-07-09-57-14.jpg>
[07/10/23, 9:57:59 AM] Prachathan Sir Pg: 6/10
[07/10/23, 9:58:28 AM] Prachathan Sir Pg: <attached: 00000098-PHOTO-2023-10-07-09-58-28.jpg>
[07/10/23, 9:58:49 AM] Prachathan Sir Pg: C/o loose stools and vomitings decreased
[07/10/23, 10:02:23 AM] Prachathan Sir Pg: <attached: 00000100-PHOTO-2023-10-07-10-02-23.jpg>
[07/10/23, 10:06:30 AM] Prachathan Sir Pg: Current problem :
Worsening renal failure with acidosis and decreased urine output
[07/10/23, 10:32:42 AM] Lohith Sir Pg Gm: Nephro opinion - advised for Hemo dialysis I/v/o severe metabolic acidosis
[07/10/23, 2:28:00 PM] Rakesh Biswas Sir GM HOD: Agree
[07/10/23, 2:30:18 PM] Rakesh Biswas Sir GM HOD: Now she appears to have developed pleural effusion. If it's due to associated heart failure it should be transudative. @919989643309 Do the ultrasound and share the video to see if she has pleural effusion
[07/10/23, 2:30:33 PM] Devendra 2018: Kk sir
[07/10/23, 3:37:45 PM] Devendra 2018: video omitted
[07/10/23, 3:40:44 PM] Rakesh Biswas Sir GM HOD: You should have also gotten someone to show where you were keeping the probe on her body
[07/10/23, 3:41:33 PM] Rakesh Biswas Sir GM HOD: The last part of the video showed the effusion very briefly but I guess it's not a lot that needs tapping
[07/10/23, 3:42:39 PM] Devendra 2018: This message was deleted.
[07/10/23, 3:42:58 PM] Devendra 2018: Okay sir
[07/10/23, 3:43:31 PM] Rakesh Biswas Sir GM HOD: Now do the video of the other patient with liver abscess asap and share in his group
[07/10/23, 3:43:54 PM] Rakesh Biswas Sir GM HOD: Hey you learned English!!! 👏👏
[07/10/23, 3:44:37 PM] Rakesh Biswas Sir GM HOD: @918790889907 's opd appears to have cleared?
[07/10/23, 3:44:46 PM] Himaja PGY1: Yes sir
[07/10/23, 3:45:11 PM] Rakesh Biswas Sir GM HOD: One upside to the new opd protocol?
[07/10/23, 3:46:01 PM] ~ Gautham: Devendra 2018 added ~ Gautham
[07/10/23, 3:46:16 PM] Himaja PGY1: Patients still has to accommodate to the new protocol they are dissatisfied currently
[07/10/23, 3:50:57 PM] Rakesh Biswas Sir GM HOD: Any change has to go through these stages, ridicule, opposition and then acceptance.
It's for their own good and everyone's good
[07/10/23, 4:00:43 PM] Rakesh Biswas Sir GM HOD: What happened to the Casualty mri patient that Prachetan was supposed to inform about
[07/10/23, 4:01:42 PM] Himaja PGY1: Mri appears to be normal sir
[07/10/23, 4:08:11 PM] Rakesh Biswas Sir GM HOD: Who wants to know that!!
We wanted to know about the patient and what's been done for her!!
[08/10/23, 12:19:19 PM] Faran: Faran joined using this group's invite link
[08/10/23, 12:19:23 PM] Faran: Make me admin
[09/10/23, 1:56:54 PM] sowmika marru: You deleted this message.
[09/10/23, 2:18:36 PM] Prachathan Sir Pg: Date- 9/10/23
ICU- bed no- 1
Unit-6
Date of admission 30/9/23
S- c/o breathlessness decreased post dialysis
O- on examination, patient is conscious, coherent, cooperative.
pallor present .
B/L lower limb pitting type edema (till Ankle)
No signs of icterus, cyanosis, clubbing, lymphadenopathy.
Vitals-
Bp- 110/80 mmhg
Temp- 99.6 F
Fever spikes present but decreased compared to yesterday
PR- 104 bpm
RR- 13 cpm
GRBS - 128 mg/dl
CVS - s1, s2 heard, no murmurs
RS - BAE present, NVBS heard
P/A- soft,non tender
Bowel sounds heard
CNS - NFND
ABG Today:
PH-7.5
Pco2-23
Po2-79
Hco3-22
Hb-6.2
TLC-6000
Plt-3L
A-
? ATYPICAL PNEUMONIA
OLIGURIC RENAL FAILURE
METABOLIC ACIDOSIS ( resolving) with
SEVERE ANEMIA
K/c/o HTN SINCE 2 YEARS
Thrombophlebitis of left hand
S/P 1 SESSION OF HEMODIALYSIS on 7/10/23.
P -
1. IV FLUIDS NS, DNS @ 50 ml/hr
2. INJ. PCM 1G IV/SOS
4.TAB. PCM 650 mg PO/QID
5.INJ. LASIX 20mg IV/BD
6.INJ. KCl 2 ampules in 500ml NS IV/STAT
7.Protein powder 2tbsp in a glass of water PO/BD
8.BP, PR ,temp monitoring 4 th hourly
Can we plan for one more session of hemodialysis today with prbc transfusion?
Sir what is the further plan of management from here
Shall we stick to the current conservative symptomatic treatment with regular vitals monitoring and the renal failure will come down gradually?
[09/10/23, 2:19:00 PM] Prachathan Sir Pg: @919100206300 share the fever chart
[09/10/23, 2:23:15 PM] Rakesh Biswas Sir GM HOD: Share the fever chart asap to allow us to understand at a glance what we have done and found differently each day since last 10 days asap
[09/10/23, 2:23:41 PM] Rakesh Biswas Sir GM HOD: Share the serial hb since admission
[09/10/23, 2:24:59 PM] Rakesh Biswas Sir GM HOD: Why hasn't she been transferred to nephro yet? Do they allow us to keep our AKI patients and get them dialyzed without transferring?
[09/10/23, 2:26:11 PM] Rakesh Biswas Sir GM HOD: Was she having CKD since last two years and no one tested her target organs even after finding her hypertensive two years back?
[09/10/23, 2:26:31 PM] Rakesh Biswas Sir GM HOD: USG kidney video
[09/10/23, 2:27:09 PM] Rakesh Biswas Sir GM HOD: Serial stool Images since admission? Daily stool volume?
[09/10/23, 2:28:08 PM] Rakesh Biswas Sir GM HOD: 👆
[09/10/23, 2:29:20 PM] Rakesh Biswas Sir GM HOD: Hb from 9.4 to 6.1 since last ten days
Maximal fall post dialysis
[09/10/23, 2:30:56 PM] Rakesh Biswas Sir GM HOD: Share the serial creatinine values since admission! Other than on 6/10 none of the other creatinine values are visible @919989643309
[09/10/23, 2:32:28 PM] Rakesh Biswas Sir GM HOD: How much was the creatinine on 1/10/23?
[09/10/23, 2:34:33 PM] Rakesh Biswas Sir GM HOD: Stool culture sent for Salmonella? Please mention Salmonella in the requisition
Oh it was asked for the other male patient with the classical pattern? What about his updates?
Although looking at this lady's chart it may not be either well represented data or it may not be Salmonella
[09/10/23, 2:34:39 PM] Prachathan Sir Pg: she is not having any structural abnormalities of kidney sir
She never got tested for renal parameters and other end organ damage in the past sir
[09/10/23, 2:35:29 PM] Rakesh Biswas Sir GM HOD: 👆
[09/10/23, 2:35:45 PM] Prachathan Sir Pg: 1.9 sir
[09/10/23, 2:35:53 PM] Rakesh Biswas Sir GM HOD: Keep the machine ready. I will do it now
[09/10/23, 2:36:02 PM] Prachathan Sir Pg: Yes sir
[09/10/23, 2:36:45 PM] Prachathan Sir Pg: Initially it was 1.9 sir
Which gradually progressed to 3.1 before dialysis
[09/10/23, 2:37:40 PM] Prachathan Sir Pg: We have sent the stool for c&s sir
Will collect the report
[09/10/23, 2:38:45 PM] Rakesh Biswas Sir GM HOD: With a respiratory rate of 13 and other stable vitals why is she in ICU? There's something missing in this data you shared that doesn't convey the criticality of her situation or is it the fact that she had worsened respiratory rate and someone doesn't know how to see it?
[09/10/23, 2:41:33 PM] sowmika marru: <attached: 00000146-PHOTO-2023-10-09-14-41-33.jpg>
[09/10/23, 2:41:56 PM] Prachathan Sir Pg: Sry sir it was 23cpm
Her tachypnea has decreased sir
She had hypotension during the dialysis even though we put on UF of zero ,so we put her on norad and gradually tapered it and stopped sir
[09/10/23, 2:42:10 PM] Prachathan Sir Pg: @919100206300 join both the charts
[09/10/23, 2:42:30 PM] sowmika marru: Yes sir
[09/10/23, 2:43:43 PM] sowmika marru: You deleted this message.
[09/10/23, 2:44:01 PM] Rakesh Biswas Sir GM HOD: 👆Add everyday's creatinine values here since admission
[09/10/23, 2:45:01 PM] Rakesh Biswas Sir GM HOD: 👆7/10 Do we have any chest X-ray after that?
[09/10/23, 2:49:30 PM] sowmika marru: You deleted this message.
[09/10/23, 2:50:22 PM] Prachathan Sir Pg: @919100206300 add these in fever chart itself
[09/10/23, 3:15:42 PM] Devendra 2018: video omitted
[09/10/23, 4:22:20 PM] Rakesh Biswas Sir GM HOD: 👆Hospital identifiers are visible!! 🧐😳
[09/10/23, 4:22:52 PM] Rakesh Biswas Sir GM HOD: 👏
[09/10/23, 4:23:14 PM] Rakesh Biswas Sir GM HOD: Share the best way to do the size calculations
[09/10/23, 4:24:55 PM] Devendra 2018: Okay sir
[09/10/23, 4:27:45 PM] sowmika marru: <attached: 00000160-PHOTO-2023-10-09-16-27-45.jpg>
[09/10/23, 4:29:59 PM] Rakesh Biswas Sir GM HOD: Can you calculate the efficacy of dialysis using the before and after creatinine values @919989643309 @919100206300
[09/10/23, 4:31:24 PM] sowmika marru: It’s already written sir
[09/10/23, 4:32:04 PM] sowmika marru: You deleted this message.
[09/10/23, 4:32:46 PM] sowmika marru: <attached: 00000164-PHOTO-2023-10-09-16-32-46.jpg>
[09/10/23, 4:32:55 PM] Rakesh Biswas Sir GM HOD: 👆
[09/10/23, 4:33:54 PM] Rakesh Biswas Sir GM HOD: All her serial chest X-rays keep changing!!
Now all of a sudden we have one that shows a cardiomegaly!
[10/10/23, 11:44:08 AM] Himaja PGY1: Date- 10/10/23
ICU- bed no- 1
Unit-6
Date of admission 30/9/23
S- subjectively feeling better and caught up better sleep
Complains of cough- productive
O- on examination, patient is conscious, coherent, cooperative.
pallor present .
B/L lower limb pitting type edema (till Ankle)
No signs of icterus, cyanosis, clubbing, lymphadenopathy.
Vitals-
Bp- 110/80 mmhg
Temp- 99.6 F
Fever spikes present but decreased compared to yesterday
PR- 104 bpm
RR- 13 cpm
GRBS - 128 mg/dl
CVS - s1, s2 heard, no murmurs
RS - BAE present, NVBS heard
P/A- soft,non tender
Bowel sounds heard
CNS - NFND
Hb-8.5
TLC- 7900
Plt-2.1
UREA - 41
CREATININE- 1.4
Na- 133
K-3.2
Cl-99
A-
? ATYPICAL PNEUMONIA
OLIGURIC RENAL FAILURE
METABOLIC ACIDOSIS ( resolving) with
SEVERE ANEMIA
K/c/o HTN SINCE 2 YEARS
Thrombophlebitis of left hand
S/P 2 SESSION OF HEMODIALYSIS with one PRBC transfusion
P -
1. IV FLUIDS NS 30ml+urine output
2. INJ. PCM 1G IV/SOS
3.INJ METHYLPREDNISOLONE 1G IV/OD
4.TAB. PCM 650 mg PO/QID
5.INJ. LASIX 20mg IV/BD if BP>110mmhg
6. TAB SODIUM BICARBONATE 500MG PO/BD
7.Protein powder 2tbsp in a glass of water PO/BD
8.BP, PR ,temp monitoring 4 th hourly
Levels of Blooms:
Level 1:Remembering
It’s all about recollecting and remembering the history of the patient.
SEPSIS SYMPTOMS-
Level 2:
Understanding:
It is all about understanding the disease pattern , it’s pathology and its associations.
STAGES OF SEPSIS-
1) Infection
2) Systemic Inflammatory Response Syndrome (SIRS)-
[SIRS criteria include two or more of the following]-
- Fever or hypothermia
- Elevated heart rate
- Rapid breathing
- Abnormal white blood cell count (high or low)
3) Sepsis-
In this stage, there may be organ dysfunction, but it's not as severe as in severe sepsis or septic shock.
4) Severe Sepsis-
Severe sepsis is characterized by organ dysfunction, often involving the heart, lungs, kidneys, liver, or blood clotting.
5) Septic Shock-
Septic shock is the most critical and life-threatening stage of sepsis. It occurs when there's a severe drop in blood pressure, which can lead to multiple organ failure.
Level 3:
Application:
It is applying the level 1 and 2 knowledge so as to provide a holistic approach of treatment to the patient.
CAUSES OF METABOLIC ACIDOSIS-
Level 4:
Analysis
Level 5
Evaluation
AKI AND CKD ?
https://www.researchgate.net/figure/Differences-between-AKI-and-CKD_tbl3_41895379
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4531835/
AKI is a sudden and often reversible decrease in kidney function, while CKD is a long-term, usually irreversible loss of kidney function. The two conditions have different causes, symptoms, and diagnostic criteria, and they require distinct approaches to treatment and management. CKD may develop as a consequence of recurrent or severe AKI, emphasizing the importance of timely management of AKI to prevent its progression.
OPD Case:
























Comments
Post a Comment